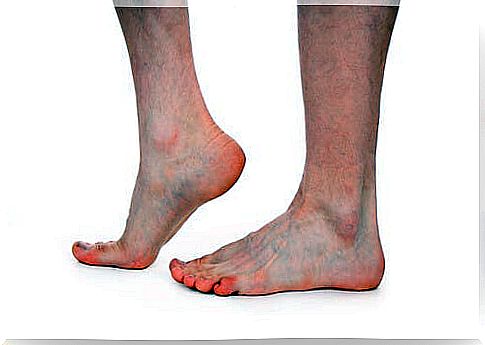
Athlete’s Foot In Children

Tinea pedis is popularly known as athlete’s foot. This is a term that can be confusing and lead to believe that it can only appear in young people and adults, mainly because of its reputation for contagion in places such as gym showers, where you are prone to touching the floor with your bare and wet feet.
However, the condition can be contracted outside of the showers, and likewise, it is not an exclusive infection of adulthood, athlete’s foot in children is also possible.
What is athlete’s foot?
Athlete’s foot is a dermatological infection that occurs between the toes.
Hence, public showers are the most common place to get infected. Not only because of the humidity, but also because of the sweat that bare feet that touch the ground can give off after exercising.

Prevention
Athlete’s foot can be spread anywhere, as long as unprotected feet make direct contact in an area contaminated with the tinea pedis fungus.
Here are some typical ways in which children get or promote the growth of athlete’s foot:
- Shower at home.
- Pools and beaches. Aquatic environments, such as swimming pools or beaches, are usually full of people who walk on the coast or around the pool without using sandals or any type of footwear. It is important to wear proper footwear when visiting these places;
- Type of footwear. Always wear comfortable shoes and socks. Some shoes or socks do not allow the skin of the feet to perspire. This produces a sauna effect, due to the trapped heat flow, which makes the foot sweat.
- Do not share a towel or sandals. It is important to have a pair of bath sandals and a personal towel, which should not be shared with others.
Symptoms of childhood athlete’s foot
Infections that affect almost exclusively the skin of the feet are very few, which is why the symptoms of athlete’s foot are very easy to deduce when an infection is discovered in this area.
Even so, it is always best to see your GP for guidance on the recommended treatment for athlete’s foot in children. Typically, the progression of athlete’s foot symptoms in children is:
- Itching sensation on the sole of the foot. It appears concomitantly with small white spots in the area of contagion. At this first point, the fungus can grow from the area of infection, or settle later in a more suitable area, such as between the toes, which tend to be more likely to retain moisture from the shower or sweat;
- The itching is later accompanied by irritation in the area where the fungus is contagious, which makes wearing footwear uncomfortable;
- The deterioration of the first layer of the epidermis of the sole of the foot begins to be noticed. In a clearer sense, that thin skin, which many call peel or skin, begins to detach or crack because the fungus is feeding on it;
- It is important that you act quickly to contain the infection in the first symptoms of its appearance. This is because the fungus can spread under the nails and cause onychomycosis, a chronic condition that causes the nails to lose their shine, look unsightly and become brittle.
Treatment of athlete’s foot in children
Athlete’s foot is treated with antifungal drugs, usually in ointment form, that kill the fungus, or stop or reverse its growth.
The fungus, like many other organisms of this class, can remain dormant and dormant for a long time, so after first developing athlete’s foot, it is important to be alert and know that it can recur. Even if adequate anti-contagion measures have been taken.
Although in both children and adults, athlete’s foot can remain dormant, it normally returns less intensely, and in many cases, even the immune system itself is capable of suppressing the growth of the fungus.